Cornea
What is the Cornea?
The cornea is the clear, dome-shaped tissue on the surface of the eye. The cornea may seem like just a clear window, but it is actually a highly organized and complex tissue. The cornea lacks blood vessels and therefore gets its nutrients from fluid in the eye (aqueous humor), and oxygen from the air in the environment.
The main purpose of the cornea is to protect the eye from injury and infection, as well as focus light onto the retina. Irregularities in the cornea are the cause of common refractive errors such as myopia, hyperopia, and astigmatism. The cornea is made up of five main layers, each with its own job.
- Epithelium: The outermost layer of the cornea, the epithelium is responsible for protecting the eye from infection and providing a smooth surface for the tear film. This layer is very thin and is constantly regenerating, like the skin on the rest of the body.
- Bowman’s layer: This extremely thin, strong layer acts as a sheet of connective tissue between the epithelium and stroma. Its dense nature protects the rest of the cornea from scratches and minor injury.
- Stroma: This layer makes up the majority (~90%) of the cornea’s thickness. It is made of strands of connective tissue called collagen fibrils. The stroma acts like a sponge, trying to absorb water from the aqueous humor inside the eye, and the tear film on the surface.
- Descemet’s membrane: This thin layer separates the stroma from the endothelial layer. This layer gradually thickens throughout life.
- Endothelium: This is the innermost layer of the cornea, and is made up of tiny cells that act like water pumps. These pump cells maintain the water content of the cornea. When the endothelium is not working properly, fluid can build up in the cornea and cause swelling, causing hazy or blurry vision.
Common Corneal Conditions
The cornea is surprisingly resilient but is still susceptible to many different conditions. Common corneal conditions include:
Corneal abrasion
Corneal abrasions refer to scratches on the surface of the eye. Small scratches that only penetrate the epithelium will usually heal without any damage to vision. If the scratch penetrates beyond the Bowman’s layer, scarring can occur, which can impact vision. Corneal abrasions can be intensely painful but usually heal quickly if there is no infection.
Fuchs Endothelial Corneal Dystrophy
Fuchs Endothelial Corneal Dystrophy is dysfunction of the corneal endothelium where the pump cells do not work well. This leads to thickening of the overlying Descemet’s membrane as well as swelling of the cornea, causing a decrease in the visual acuity and quality. This can also cause blisters to form underneath the epithelium; like skin blisters, these can be quite painful when they rupture.
Corneal Ulcer
This is a corneal abrasion that becomes infected. Typically, antibiotics are used to kill the infection, allowing the cornea to heal itself. If an ulcer is dealt with quickly, there is a good chance the impact on long-term vision will be minimal.
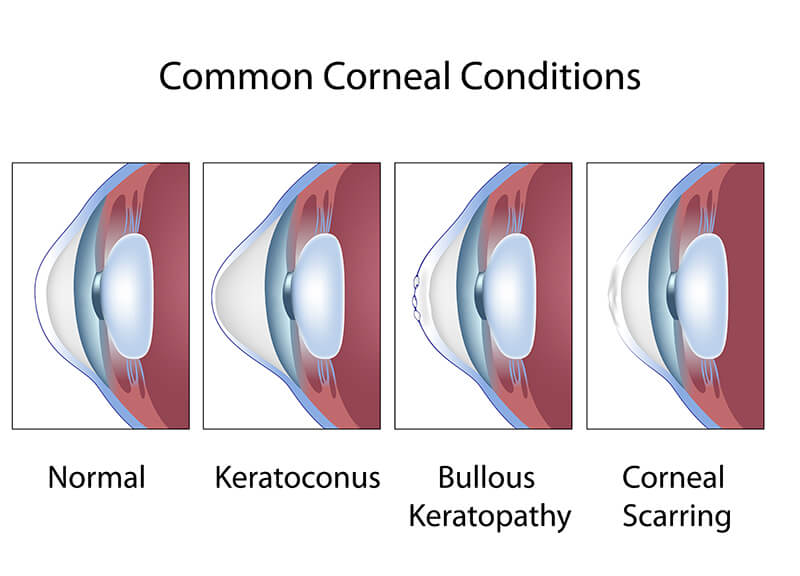
Bullous Keratopathy
Bullous Keratopathy is a dysfunction of the corneal endothelium caused by previous injury or surgery. This leads to swelling of the cornea causing a decrease in the visual acuity and quality. The corneal swelling can sometimes become severe and cause blisters on the epithelium which can be painful and increase the risk for infection.
Dry eyes
Dry eye syndrome is one of the most common conditions in the US. Dry eye syndrome causes red, irritated, itchy and dry feeling eyes. This is commonly due to a decrease in tear production or blepharitis/meibomian gland dysfunction, which causes poor tear quality.
Keratoconus
Keratoconus is a progressive corneal dystrophy. In patients with keratoconus, the cornea begins to take on a cone-like shape and bulges forward. This causes extremely blurry vision and gets worse over time. Keratoconus patients are usually young, typically in their teens or twenties, and typically rub their eyes frequently. For Keratoconus, that is progressively worsening, there is a treatment known as Corneal Cross-linking (sometimes called CXL or KXL).
Pterygium
This is caused by an abnormal (although non-cancerous) growth of tissue from the white part of the eye (conjunctiva) that has grown towards the center of the cornea. A pterygium can enlarge over time, progressively obscuring the vision. When small, they can be watched for years but can be removed surgically if large enough to interfere with vision.
Corneal Procedures Available at Georgia Eye Associates
Here at Georgia Eye Associates, we take pride in offering the best corneal procedures available. Our very own Dr. Strauss is one of very few doctors in the state of Georgia to perform these corneal procedures. Dr. Strauss specializes in different types of corneal transplants. These procedures include:
- PKP – Penetrating keratoplasty (PKP) is the traditional full-thickness corneal transplant. Often performed on patients with corneal scars or advanced keratoconus, this procedure is usually a last resort. While this procedure is performed often and is considered safe and effective, recovery time can be long. There is also greater risk of tissue rejection than with other corneal transplants.
- DALK – Deep anterior lamellar keratoplasty (DALK) is a newer type of corneal transplant. During this procedure, the anterior (outer) portion of the cornea is replaced with donor tissue, leaving the inner layers (the endothelium) alone. Because the inner layer is retained, there is less risk of rejection.
- DMEK – Descemet’s membrane endothelial keratoplasty (DMEK) is a type of partial-thickness corneal transplant. During this procedure, the Descemet’s membrane and endothelium are removed and replaced with thin donor tissue consisting of only Descemet’s and endothelium. This is a delicate procedure but ensures faster recovery time and less risk of graft rejection compared to a penetrating keratoplasty. The final visual outcome is often slightly better with DMEK as opposed to DSEK.
- DSEK – Descemet’s stripping endothelial keratoplasty (DSEK) is a type of partial-thickness corneal transplant. During this procedure, Descemet’s membrane and endothelium are removed and replaced with donor tissue consisting of a small amount of corneal stroma, Descemet’s membrane, and endothelium. This ensures faster recovery time and less risk of graft rejection compared to a penetrating keratoplasty. DSEK is an excellent choice for eyes that have had multiple surgeries or trauma, where DMEK may be too difficult to perform.
- Pterygium removal – The abnormal tissue from the conjunctiva is removed, along with the portion of tissue that has grown onto the cornea. A piece of donor tissue is then used to cover the gap in the conjunctival tissue. When done appropriately, the risk of recurrence of the pterygium is quite low.






